DIABETES, FOOT HEALTH AND THE ROLE OF PODIATRY
National Diabetes Week is a crucial time to raise awareness about the effects, prevention and management of this devastating condition. Diabetes is a complex disorder that affects many organs, of which the feet are particularly susceptible. According to Diabetes Australia, diabetes is the epidemic of the 21st century, with:
– 280 Australians developing diabetes every day… that’s 1 person every 5 minutes;
– 1.7 million Australians currently living with diabetes, of which it’s estimated 500,000 don’t know it;
– 4,400 amputations occuring every year in Australia as a result of diabetes.
With foot-related complications being so prevalent, the role of podiatry is crucial in the management of this disease. That’s why our podiatrists are committed to educating our patients, and the wider community, so that the physical, social and monetary costs associated with this disease can be can reduced.
What is Diabetes?
Diabetes is a complex condition. It is important to understand that although there are several types of diabetes; all have the potential to be serious and affect the entire body in different ways.
Glucose is a form of sugar that is an essential source of energy for our bodies. Put simply, when one develops diabetes, they are unable to maintain healthy levels of glucose in their blood. Insulin is a hormone that helps convert glucose into energy, this is an essential process of the body to help it function normally. People living with diabetes tend to no longer produce, or produce insufficient amounts of, insulin.
Therefore, when people with diabetes consume certain foods that contain glucose (fruit, sweets and starchy vegetables for example) they’re unable to convert it into energy. As a result, glucose remains in the blood and their blood glucose levels become high.
The main types of diabetes are type 1, type 2 and gestational diabetes, with no-one being immune to developing diabetes.
Complications associated with Diabetes
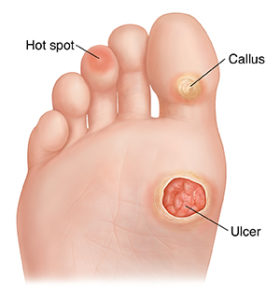
Foot health complications can include:
– Changes to skin integrity (dry, cracked skin)
– Changes in structure of the feet
– Compromised blood supply to the feet
– Loss of the ability to feel the feet (nerve damage)
– Inability to heal wounds
– Limb amputation
Other possible major complications of uncontrolled diabetes include:
– Stroke and heart disease
– Kidney disease
– Blindness
– Depression and anxiety
How can Podiatrists help?
Podiatrists are experts in the prevention and management of diabetes-related foot complications. As part of a Diabetes assessment, your podiatrist will conduct a:
Vascular assessment:
– Any history of vascular symptoms such as cramping leg pain that develops whilst walking and stops with rest is noted;
– All foot pulses will be palpated to assess the quality of blood flow to the feet;
– Any signs of venous problems (oedema, varicose veins) will be recorded;
– If needed, a referral to a vascular specialist may be advised.
Adequate blood supply to the feet is vital. Poor circulation can result in slow healing of wounds/cuts or the inability to heal. If a wound is unable to heal then amputation may be necessary.

Neurological assessment:
– Any history of neurological symptoms such as burning, numbness or pins and needle in the feet will be noted;
– Monofilaments and tuning forks will be used to assess your light touch, vibration and protective sensation.
It is important to have good sensation when it comes to your feet. Diminished, or a lack of sensation, can hinder your ability to feel trauma (a rock in your shoe/extreme heat). If you don’t feel, you are unable to prevent trauma from happening and are more inclined to acquire cuts, burns or wounds to the feet.

Biomechanical assessment:
– Foot structure and walking patterns will be assessed to look for areas of high pressure or foot/toe deformities.
Toe and foot deformities can be high risk areas for increased pressure. This may result in the formation of corns and calluses, which in the case of people with diabetes, can lead to wounds. Should this be the case, podiatrists can attend to any pressure lesions/wounds and implement steps to reduce this pressure via padding, footwear modifications and/or orthotics.
Footwear assessment:
– Footwear is assessed to observe any abnormal wear patterns or abnormalities.
– The inside and outside of the shoe will be checked to ensure it provides for enough support and shock absorption.
– The width and depth of the shoe is checked to ensure they fit correctly and comply with the ideal features of a diabetic shoe.
Inappropriate footwear can be a very common source of trauma in patients living with diabetes. Importantly, they are checked to prevent wound formation.
How often should you see a podiatrist?
A diabetes assessment should be conducted at least once every 12 months. However, depending on your risk profile for developing foot complications, this might be completed on a more regular basis (every 3-6 months).
Nail and skin care are also an important reason to visit a podiatrist outside these times. Incorrect cutting of nails or dry skin/fissures are ways that infections can occur in people with diabetes, so it is best to let a professional do this. Most people benefit from seeing a podiatrist every 8-10 weeks to reduce the likelihood of developing foot complications.
Tips to prevent foot complications
As there is currently no existing cure for diabetes it is important for individuals WITHOUT diabetes to maintain blood glucose levels between 4.0 and 7.8 mmol/L. If you have diabetes, your GP will advise you of your individual target range. Regular checking of your blood glucose levels enables you to act fast if any changes arise.
Here are some additional tips to help you prevent diabetes related-foot complications:
– Daily foot checks
Take particular care to note any cuts or red skin.
Use a mirror under the feet if you have trouble seeing.
– Keep your feet clean
Together with washing your feet in warm water, be sure to dry them thoroughly. Pay close attention to between the toes.
– Moisturise!
Keep your skin soft and supple.
Apply a cream or lotion on the bottom and tops of your feet (avoiding between the toes).
– Avoid being bare-foot
Always check shoes prior to wearing them to ensure they fit well and that there are no objects inside.
– Protect your feet from the heat and extreme cold
Avoid use of electric blankets
Keep feet away from heaters
Wear protective gear when at the beach/ or on hot pavements
Wear socks to warm the feet
– Keep active and maintain a healthy diet
Any movement is better than none. Be sure to keep that blood flowing to your feet!
Eating well will also assist in keeping blood glucose levels at a normal level.

If you have Diabetes, or any other foot and ankle condition that needs assessment, make an appointment by calling 94805522 or book online via our “Book Now” tab.
by Milka Trifkovic
3